Parkside’s Innovative Approach to Chronic Disease Management: A Community-Based Model
Chronic diseases are a leading cause of death and disability worldwide, placing a significant burden on healthcare systems and individuals alike. In response to this growing challenge, Parkside, a forward-thinking community, has implemented an innovative, community-based approach to chronic disease management. This model focuses on prevention, early detection, and comprehensive care, aiming to improve the quality of life for residents living with chronic conditions. This article will delve into the key components of Parkside’s strategy and explore its potential as a blueprint for other communities facing similar health challenges.
Understanding the Chronic Disease Landscape
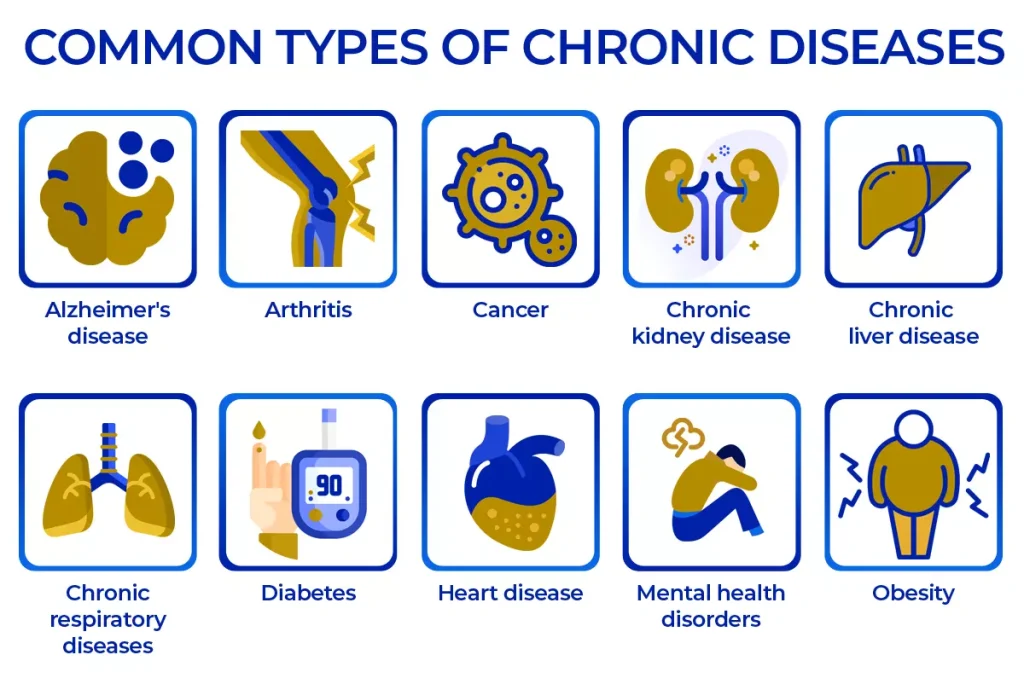
Before examining Parkside’s approach, it’s crucial to understand the scope of the chronic disease problem. Chronic diseases, such as heart disease, stroke, cancer, type 2 diabetes, and chronic respiratory diseases, are long-lasting conditions that generally progress slowly. They are often preventable through lifestyle modifications, such as adopting a healthy diet, engaging in regular physical activity, and avoiding tobacco use. However, once developed, chronic diseases require ongoing medical attention and can significantly impact an individual’s daily life.
The prevalence of chronic disease is increasing globally, driven by factors such as aging populations, urbanization, and changes in lifestyle. In the United States, for example, six in ten adults have a chronic disease, and four in ten have two or more. This highlights the urgent need for effective strategies to prevent and manage these conditions.
Parkside’s Integrated Approach to Chronic Disease Management
Parkside’s approach to chronic disease management is built on a foundation of community engagement, integrated healthcare services, and a focus on individual empowerment. The core elements of this model include:
Community Outreach and Education
Parkside recognizes that prevention is key to reducing the burden of chronic disease. The community invests heavily in outreach programs designed to educate residents about healthy lifestyles and risk factors for common chronic conditions. These programs include:
- Health fairs and screenings: Regular health fairs offer free screenings for blood pressure, cholesterol, blood sugar, and other key indicators of chronic disease risk.
- Educational workshops: Workshops on topics such as nutrition, exercise, stress management, and smoking cessation are offered throughout the year.
- Community gardens: Parkside encourages residents to grow their own fruits and vegetables through community gardens, promoting healthy eating habits and physical activity.
- Public health campaigns: Targeted campaigns address specific health issues, such as diabetes prevention or heart health awareness.
Integrated Healthcare Services
Parkside’s healthcare system is designed to provide seamless, coordinated care for individuals with chronic disease. This includes:
- Primary care providers: Primary care physicians serve as the central point of contact for patients, providing comprehensive care and coordinating referrals to specialists.
- Specialty clinics: Specialized clinics offer advanced care for specific chronic diseases, such as cardiology, endocrinology, and pulmonology.
- Care management programs: Care managers work with patients to develop personalized care plans, coordinate appointments, and provide ongoing support.
- Telehealth services: Telehealth allows patients to access care remotely, improving convenience and reducing barriers to access.
- Mental health services: Recognizing the link between mental and physical health, Parkside provides access to mental health professionals who can help patients manage stress, anxiety, and depression.
Individual Empowerment and Self-Management
Parkside’s model emphasizes empowering individuals to take control of their health. This includes:
- Self-management education: Patients with chronic disease receive education and training on how to manage their condition effectively, including monitoring symptoms, taking medications, and making lifestyle changes.
- Support groups: Support groups provide a forum for patients to connect with others who share similar experiences, fostering a sense of community and reducing feelings of isolation.
- Health coaching: Health coaches work with patients to set goals, develop strategies for behavior change, and provide ongoing motivation and support.
- Access to resources: Parkside provides access to a wide range of resources, including online information, educational materials, and community programs.
The Role of Technology in Parkside’s Approach
Technology plays a crucial role in Parkside’s chronic disease management strategy. Electronic health records (EHRs) allow healthcare providers to access patient information quickly and easily, improving care coordination and reducing the risk of errors. Telehealth services expand access to care, particularly for patients in rural areas or those with mobility limitations. Mobile health (mHealth) apps provide patients with tools to track their health, manage their medications, and communicate with their healthcare providers.
For example, Parkside utilizes a secure patient portal where individuals can view their lab results, schedule appointments, and send messages to their care team. They also employ remote patient monitoring devices for individuals with conditions like heart failure or diabetes, allowing providers to track vital signs and intervene proactively if necessary. [See also: Remote Patient Monitoring for Chronic Conditions: A Comprehensive Guide]
Measuring the Impact of Parkside’s Model
Parkside continuously monitors the impact of its chronic disease management program through a variety of metrics, including:
- Prevalence of chronic diseases: Tracking the prevalence of common chronic diseases over time to assess the effectiveness of prevention efforts.
- Hospitalization rates: Monitoring hospitalization rates for chronic disease-related complications to assess the effectiveness of care management programs.
- Emergency department visits: Tracking emergency department visits for chronic disease-related issues to identify areas where care can be improved.
- Patient satisfaction: Measuring patient satisfaction with the quality of care received through surveys and feedback mechanisms.
- Healthcare costs: Analyzing healthcare costs associated with chronic disease management to assess the cost-effectiveness of the program.
Initial data suggests that Parkside’s approach is yielding positive results. The community has seen a decrease in hospitalization rates for heart failure and diabetes, as well as improvements in patient satisfaction scores. Further research is underway to fully evaluate the long-term impact of the program.
Challenges and Opportunities
While Parkside’s model shows promise, it also faces challenges. One challenge is ensuring equitable access to care for all residents, regardless of socioeconomic status or geographic location. Another challenge is sustaining the program over time, given the ongoing need for funding and resources. [See also: Addressing Healthcare Disparities in Chronic Disease Management]
Despite these challenges, Parkside’s approach presents significant opportunities. By demonstrating the effectiveness of community-based chronic disease management, Parkside can serve as a model for other communities seeking to improve the health of their residents. The program can also be expanded to address other health issues, such as mental health and substance abuse.
Lessons Learned and Future Directions
Parkside’s experience offers valuable lessons for other communities interested in implementing similar programs. Key takeaways include:
- Community engagement is essential: Engaging residents in the design and implementation of the program is crucial for its success.
- Integrated care is key: Coordinating care across different healthcare settings is essential for providing comprehensive and effective care.
- Individual empowerment is vital: Empowering individuals to take control of their health is key to improving outcomes.
- Technology can enhance care: Technology can be used to improve access to care, enhance care coordination, and empower patients.
- Data-driven decision-making is crucial: Continuously monitoring the impact of the program and using data to inform decision-making is essential for its success.
Looking ahead, Parkside plans to further refine its chronic disease management program by incorporating new technologies, expanding its outreach efforts, and strengthening its partnerships with community organizations. The goal is to create a healthier, more vibrant community for all residents. As the prevalence of chronic disease continues to rise, innovative approaches like Parkside’s will be essential for improving the health and well-being of populations worldwide. The integrated approach to chronic disease management in Parkside serves as an example of how localized community-based programs can make a significant impact on public health.
