Does Atorvastatin Cause Liver Damage? A Comprehensive Look
Atorvastatin, a widely prescribed medication belonging to the statin family, is primarily used to lower cholesterol levels and reduce the risk of cardiovascular events like heart attacks and strokes. While atorvastatin is generally considered safe and effective, concerns about its potential side effects, particularly liver damage, often arise. This article delves into the relationship between atorvastatin and liver health, examining the evidence, risks, and necessary precautions. Understanding whether atorvastatin cause liver damage is crucial for both patients and healthcare providers to make informed decisions regarding treatment and monitoring.
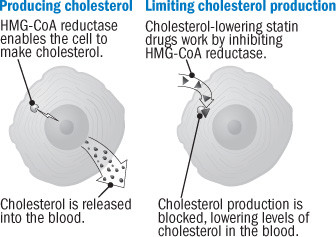
Understanding Atorvastatin and Its Mechanism of Action
Atorvastatin works by inhibiting an enzyme called HMG-CoA reductase, which is essential for cholesterol production in the liver. By blocking this enzyme, atorvastatin reduces the amount of cholesterol produced, leading to lower levels of LDL (bad) cholesterol in the bloodstream. Lowering LDL cholesterol helps prevent the buildup of plaque in the arteries, reducing the risk of heart disease. Atorvastatin is available under various brand names, including Lipitor, and is typically taken orally once daily.
The Liver’s Role in Cholesterol Metabolism
The liver plays a central role in cholesterol metabolism. It not only produces cholesterol but also processes and excretes it. Therefore, any medication that affects cholesterol metabolism, like atorvastatin, can potentially impact liver function. It is essential to understand how atorvastatin interacts with the liver to assess the risk of liver damage.
Evidence Linking Atorvastatin to Liver Damage
While atorvastatin can affect liver function, clinically significant liver damage is relatively rare. Most patients taking atorvastatin experience mild and transient elevations in liver enzymes, specifically alanine aminotransferase (ALT) and aspartate aminotransferase (AST). These enzymes are indicators of liver inflammation or damage. However, significant liver injury, such as drug-induced hepatitis or liver failure, is uncommon.
Clinical Trial Data
Clinical trials have shown that persistent and marked elevations in liver enzymes (more than three times the upper limit of normal) occur in less than 2% of patients taking atorvastatin. These elevations are often reversible upon discontinuation of the medication. However, it’s crucial to monitor liver enzyme levels regularly, especially during the initial months of treatment.
Post-Market Surveillance
Post-market surveillance studies, which analyze data from a larger and more diverse population, have also reported rare cases of severe liver injury associated with atorvastatin use. These cases are often linked to pre-existing liver conditions, alcohol abuse, or the use of other medications that can affect the liver. It is important to note that correlation does not equal causation, and further investigation is often needed to confirm the direct link between atorvastatin and severe liver damage.
Risk Factors for Atorvastatin-Induced Liver Damage
Certain factors can increase the risk of atorvastatin-induced liver damage. Identifying these risk factors is crucial for healthcare providers to assess patient suitability for atorvastatin therapy and implement appropriate monitoring strategies.
- Pre-existing Liver Conditions: Patients with pre-existing liver diseases, such as hepatitis, cirrhosis, or non-alcoholic fatty liver disease (NAFLD), are at a higher risk of developing liver damage while taking atorvastatin.
- Alcohol Abuse: Excessive alcohol consumption can exacerbate the effects of atorvastatin on the liver. Individuals who consume large amounts of alcohol regularly should exercise caution when taking atorvastatin.
- Drug Interactions: Certain medications can interact with atorvastatin and increase the risk of liver damage. These include some antibiotics, antifungals, and other cholesterol-lowering drugs. [See also: Statin Drug Interactions]
- Age: Older adults may be more susceptible to the adverse effects of atorvastatin on the liver due to age-related changes in liver function.
- High Doses of Atorvastatin: Higher doses of atorvastatin may increase the risk of liver damage compared to lower doses.
Symptoms of Liver Damage
Recognizing the symptoms of liver damage is essential for early detection and prompt medical intervention. Patients taking atorvastatin should be aware of the following signs and symptoms:
- Jaundice: Yellowing of the skin and eyes
- Dark Urine: Abnormally dark-colored urine
- Pale Stools: Light-colored or clay-colored stools
- Abdominal Pain: Pain or discomfort in the upper right abdomen
- Nausea and Vomiting: Persistent nausea and vomiting
- Fatigue: Unexplained and persistent fatigue
- Loss of Appetite: Significant decrease in appetite
If any of these symptoms occur, patients should immediately consult their healthcare provider for evaluation.
Monitoring Liver Function During Atorvastatin Therapy
Regular monitoring of liver function is crucial for patients taking atorvastatin. This typically involves periodic blood tests to measure liver enzyme levels (ALT and AST). The frequency of monitoring may vary depending on individual risk factors and the healthcare provider’s recommendations.
Baseline Liver Function Tests
Before starting atorvastatin therapy, a baseline liver function test is recommended to establish a reference point. This helps identify any pre-existing liver abnormalities and allows for a more accurate assessment of changes during treatment.
Periodic Monitoring
After initiating atorvastatin therapy, liver enzyme levels are typically monitored every 6 to 12 weeks for the first few months. If liver enzyme levels remain stable, the frequency of monitoring may be reduced. However, if significant elevations occur, further investigation and possible dose adjustment or discontinuation of atorvastatin may be necessary.
Alternative Cholesterol-Lowering Medications
For patients who experience liver damage while taking atorvastatin or have risk factors that make atorvastatin unsuitable, alternative cholesterol-lowering medications may be considered. These include:
- Other Statins: Different statins may have varying effects on liver function. Switching to a different statin, such as rosuvastatin or pravastatin, may be an option.
- Ezetimibe: Ezetimibe works by inhibiting the absorption of cholesterol in the small intestine. It can be used alone or in combination with a statin.
- Bile Acid Sequestrants: These medications bind to bile acids in the intestine, preventing their reabsorption and promoting the excretion of cholesterol.
- PCSK9 Inhibitors: PCSK9 inhibitors are injectable medications that significantly lower LDL cholesterol levels. They are typically reserved for patients who do not respond adequately to statins or have a high risk of cardiovascular events. [See also: PCSK9 Inhibitors and Heart Health]
The choice of alternative medication should be made in consultation with a healthcare provider, considering individual factors such as medical history, risk factors, and treatment goals.
Lifestyle Modifications for Liver Health
In addition to medication, lifestyle modifications can play a significant role in maintaining liver health and reducing the risk of liver damage. These include:
- Healthy Diet: A balanced diet rich in fruits, vegetables, and whole grains can support liver function. Limiting the intake of saturated and trans fats, as well as processed foods, is also beneficial.
- Regular Exercise: Regular physical activity can improve liver health and reduce the risk of non-alcoholic fatty liver disease (NAFLD).
- Moderate Alcohol Consumption: Limiting alcohol consumption or abstaining from alcohol can reduce the risk of alcohol-related liver damage.
- Weight Management: Maintaining a healthy weight can prevent and manage NAFLD.
- Avoidance of Toxins: Minimizing exposure to environmental toxins and chemicals can protect the liver from damage.
Conclusion
While atorvastatin is a valuable medication for lowering cholesterol and reducing the risk of cardiovascular events, concerns about its potential to cause liver damage are valid. Clinically significant liver damage is rare, but mild elevations in liver enzymes are more common. Regular monitoring of liver function is crucial, especially in patients with pre-existing liver conditions or other risk factors. Patients should be aware of the symptoms of liver damage and promptly report any concerns to their healthcare provider. Alternative cholesterol-lowering medications and lifestyle modifications can also be considered to manage cholesterol levels and protect liver health. Understanding the risks and benefits of atorvastatin allows for informed decision-making and optimal patient care. The question of whether atorvastatin cause liver damage is complex, and a thorough evaluation by a healthcare professional is always recommended to ensure patient safety and well-being.
