Bisphosphonates: Understanding Their Uses, Benefits, and Potential Risks
Bisphosphonates are a class of drugs primarily used to prevent and treat bone loss. They are a cornerstone in managing conditions like osteoporosis, Paget’s disease of bone, and bone metastases from cancer. Understanding how bisphosphonates work, their benefits, and potential side effects is crucial for both patients and healthcare providers. This article delves into the intricacies of bisphosphonates, providing a comprehensive overview of their uses, efficacy, and safety profile.
What are Bisphosphonates?
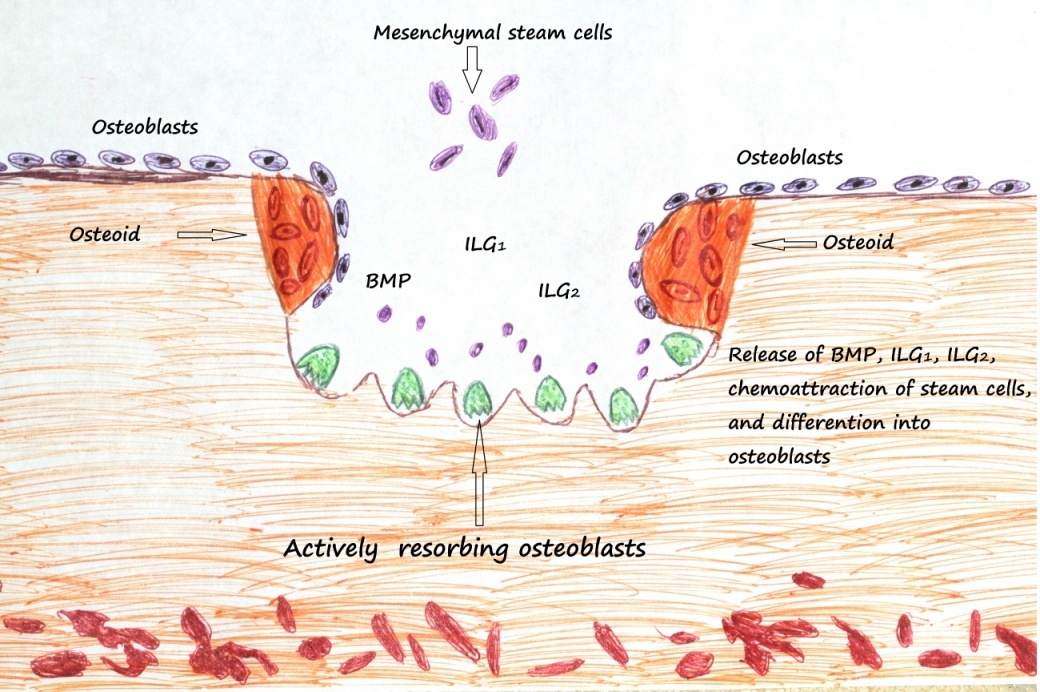
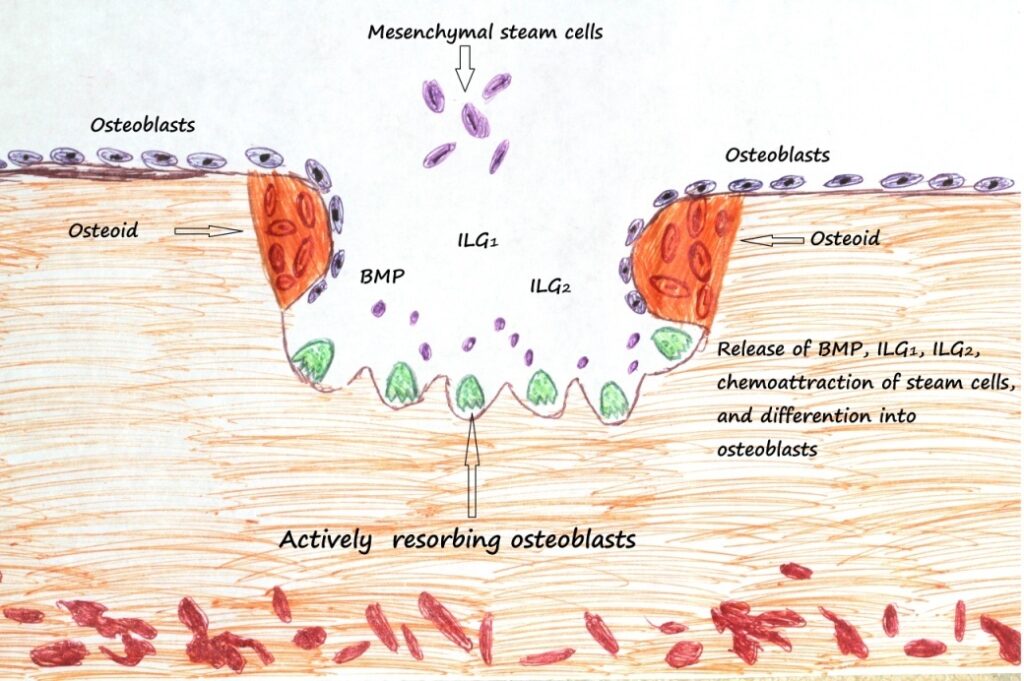
Bisphosphonates are synthetic analogs of pyrophosphate, a naturally occurring substance in the body that regulates bone turnover. Bone turnover is a continuous process where old bone is broken down (resorption) and new bone is formed (formation). In conditions like osteoporosis, bone resorption exceeds bone formation, leading to weakened bones and increased fracture risk. Bisphosphonates work by inhibiting osteoclasts, the cells responsible for bone resorption. By slowing down the breakdown of bone, bisphosphonates help to increase bone density and reduce the risk of fractures.
Types of Bisphosphonates
Bisphosphonates are available in various forms and potencies, broadly categorized into oral and intravenous (IV) formulations. Some common bisphosphonates include:
- Alendronate (Fosamax): An oral bisphosphonate commonly prescribed for osteoporosis.
- Risedronate (Actonel): Another oral bisphosphonate used for osteoporosis and Paget’s disease.
- Ibandronate (Boniva): Available in both oral and IV formulations, primarily used for osteoporosis in women.
- Zoledronic acid (Reclast): An IV bisphosphonate administered once yearly for osteoporosis and also used for other bone-related conditions.
- Pamidronate (Aredia): An IV bisphosphonate used to treat hypercalcemia of malignancy and bone metastases.
- Etidronate (Didronel): An older bisphosphonate used for Paget’s disease and heterotopic ossification.
The choice of bisphosphonate depends on factors such as the patient’s condition, severity of bone loss, tolerance, and convenience.
How Bisphosphonates Work
Bisphosphonates selectively accumulate in bone, particularly at sites of active bone resorption. Once internalized by osteoclasts, they disrupt the cells’ function, leading to their apoptosis (programmed cell death) or reduced activity. This inhibition of osteoclasts reduces the rate of bone resorption, allowing bone formation to catch up and ultimately increasing bone density. Different bisphosphonates have varying potencies and mechanisms of action, contributing to their specific clinical applications.
Conditions Treated with Bisphosphonates
Bisphosphonates are primarily used to treat and prevent conditions characterized by excessive bone loss:
Osteoporosis
Osteoporosis is a condition characterized by low bone density and increased risk of fractures. Bisphosphonates are a first-line treatment for osteoporosis, significantly reducing the risk of vertebral and non-vertebral fractures. They are effective in both postmenopausal women and men with osteoporosis. [See also: Osteoporosis Management Strategies]
Paget’s Disease of Bone
Paget’s disease is a chronic disorder that disrupts the normal bone remodeling process, leading to enlarged and weakened bones. Bisphosphonates are used to normalize bone turnover and reduce pain associated with Paget’s disease.
Bone Metastases
Bone metastases occur when cancer cells spread to the bones from other parts of the body. Bisphosphonates can help to reduce pain, prevent fractures, and decrease the need for radiation therapy in patients with bone metastases from cancers such as breast cancer, prostate cancer, and multiple myeloma.
Hypercalcemia of Malignancy
Hypercalcemia of malignancy is a condition where cancer cells release substances that cause high levels of calcium in the blood. Bisphosphonates can help to lower calcium levels and alleviate symptoms associated with hypercalcemia.
Other Uses
Bisphosphonates are also used in other conditions such as osteogenesis imperfecta (brittle bone disease) and fibrous dysplasia.
Benefits of Bisphosphonates
The primary benefit of bisphosphonates is their ability to reduce the risk of fractures in individuals with osteoporosis and other bone-related conditions. Clinical trials have demonstrated significant reductions in vertebral, hip, and non-vertebral fractures with bisphosphonate therapy. Additionally, bisphosphonates can improve bone pain, reduce the need for pain medication, and enhance quality of life in patients with bone metastases and Paget’s disease.
Potential Risks and Side Effects
While bisphosphonates are generally safe and effective, they can be associated with certain risks and side effects. It’s important to weigh the benefits against the potential risks before starting bisphosphonate therapy.
Common Side Effects
Common side effects of oral bisphosphonates include:
- Gastrointestinal issues: Heartburn, acid reflux, nausea, abdominal pain, and diarrhea. Taking oral bisphosphonates with a full glass of water and remaining upright for at least 30 minutes can help to minimize these side effects.
- Flu-like symptoms: Some patients experience flu-like symptoms such as fever, chills, muscle aches, and fatigue, particularly after the first dose of an IV bisphosphonate.
Rare but Serious Side Effects
Rare but serious side effects of bisphosphonates include:
- Osteonecrosis of the jaw (ONJ): ONJ is a rare condition characterized by the death of bone tissue in the jaw. It is more common in patients receiving high doses of IV bisphosphonates for cancer treatment. Good oral hygiene and regular dental checkups can help to reduce the risk of ONJ.
- Atypical femur fractures: Long-term use of bisphosphonates has been associated with an increased risk of atypical femur fractures, which are fractures that occur in the upper part of the thigh bone and have a distinct pattern.
- Esophageal problems: Oral bisphosphonates can irritate the esophagus and, in rare cases, cause esophagitis, esophageal ulcers, or esophageal strictures.
- Atrial fibrillation: Some studies have suggested a possible association between bisphosphonate use and an increased risk of atrial fibrillation, an irregular heart rhythm.
Precautions and Contraindications
Bisphosphonates are not suitable for everyone. They should be used with caution in patients with:
- Kidney problems: Bisphosphonates are cleared from the body by the kidneys, so they should be used with caution in patients with impaired kidney function.
- Esophageal disorders: Patients with esophageal disorders such as Barrett’s esophagus or esophageal strictures should avoid oral bisphosphonates.
- Hypocalcemia: Bisphosphonates can lower calcium levels in the blood, so they should not be used in patients with hypocalcemia.
- Pregnancy and breastfeeding: Bisphosphonates are not recommended during pregnancy and breastfeeding.
How to Take Bisphosphonates
The instructions for taking bisphosphonates vary depending on the specific medication and formulation. However, some general guidelines include:
- Oral bisphosphonates: Take on an empty stomach with a full glass of water at least 30 minutes before eating or taking other medications. Remain upright for at least 30 minutes after taking the medication.
- IV bisphosphonates: Administered by a healthcare professional via intravenous infusion. The frequency of infusions varies depending on the medication.
It’s important to follow the specific instructions provided by your healthcare provider and pharmacist.
Alternatives to Bisphosphonates
For individuals who cannot tolerate or are not suitable for bisphosphonates, alternative treatments for osteoporosis include:
- Denosumab (Prolia): A monoclonal antibody that inhibits bone resorption.
- Teriparatide (Forteo) and Abaloparatide (Tymlos): Anabolic agents that stimulate new bone formation.
- Raloxifene (Evista): A selective estrogen receptor modulator (SERM) that has estrogen-like effects on bone.
- Estrogen therapy: Can help to prevent bone loss in postmenopausal women.
Lifestyle modifications such as regular exercise, a calcium-rich diet, and vitamin D supplementation are also important for maintaining bone health.
The Future of Bisphosphonates
Research continues to explore new uses and formulations of bisphosphonates. Scientists are investigating ways to improve the efficacy and safety of these medications, as well as to develop new treatments for bone-related conditions. Ongoing studies are also examining the long-term effects of bisphosphonate therapy and the optimal duration of treatment. [See also: Emerging Therapies for Bone Health]
Conclusion
Bisphosphonates are a valuable tool in the prevention and treatment of bone loss. They can significantly reduce the risk of fractures and improve the quality of life for individuals with osteoporosis, Paget’s disease, and bone metastases. However, like all medications, bisphosphonates are associated with potential risks and side effects. It’s important to discuss the benefits and risks with your healthcare provider to determine if bisphosphonate therapy is right for you. Understanding the nuances of bisphosphonate treatment empowers patients to make informed decisions and optimize their bone health.