Navigating Medicaid NYRx: A Comprehensive Guide to New York’s Pharmacy Program
Medicaid NYRx, New York’s Medicaid pharmacy program, is a critical component of the state’s healthcare system, ensuring access to necessary prescription medications for eligible individuals. Understanding how Medicaid NYRx functions, its eligibility criteria, covered medications, and recent changes is essential for both beneficiaries and healthcare providers. This article provides a comprehensive overview of Medicaid NYRx, offering clarity and guidance through its complexities.
Understanding Medicaid NYRx
Medicaid NYRx is the pharmacy benefit program under New York’s Medicaid program. It covers prescription drugs and certain over-the-counter medications prescribed by a healthcare provider. The program aims to provide affordable access to medications for low-income individuals, families, seniors, and people with disabilities who qualify for Medicaid in New York State. The program’s administration involves a network of participating pharmacies and managed care organizations (MCOs) that work together to deliver these vital services.
The program’s primary goal is to ensure that eligible individuals have access to the medications they need to manage their health conditions effectively. By providing comprehensive pharmacy benefits, Medicaid NYRx helps to improve health outcomes, reduce hospitalizations, and enhance the overall quality of life for its beneficiaries. The program is continually evolving to meet the changing healthcare needs of New Yorkers, with ongoing adjustments to its formulary, policies, and procedures.
Eligibility for Medicaid NYRx
To be eligible for Medicaid NYRx, individuals must first qualify for New York State Medicaid. Medicaid eligibility is based on several factors, including income, household size, age, disability status, and immigration status. Specific income thresholds and asset limits apply, and these can vary depending on the category of Medicaid coverage sought. Generally, individuals with lower incomes and limited resources are more likely to qualify.
Children, pregnant women, seniors, and individuals with disabilities often have different eligibility criteria than other adults. For example, children and pregnant women may be eligible for Medicaid even if their family income exceeds the standard limits. Similarly, seniors and individuals with disabilities may qualify for Medicaid through programs that consider both income and medical expenses. It’s crucial to consult the New York State Department of Health or a local Medicaid office for precise eligibility requirements and application procedures.
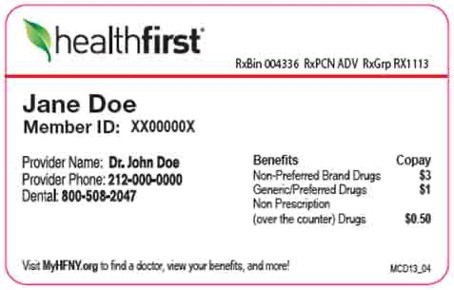
Once an individual is enrolled in Medicaid, they automatically become eligible for Medicaid NYRx. There is no separate application process for the pharmacy benefit program. Enrollees can access prescription medications at participating pharmacies by presenting their Medicaid card and a valid prescription from a healthcare provider.
Covered Medications under Medicaid NYRx
Medicaid NYRx covers a wide range of prescription medications, including brand-name and generic drugs. The program maintains a formulary, which is a list of preferred medications that are covered without prior authorization. The formulary is regularly updated to reflect new medications, changes in clinical guidelines, and cost considerations. Beneficiaries and healthcare providers can access the formulary online or through their Medicaid managed care organization.
While the formulary includes a comprehensive selection of medications, some drugs may require prior authorization before they can be covered. Prior authorization is a process in which the healthcare provider must obtain approval from Medicaid NYRx before prescribing certain medications. This is typically required for drugs that are more expensive, have potential safety concerns, or are used for specific conditions. The prior authorization process helps to ensure that medications are used appropriately and cost-effectively.
In addition to prescription drugs, Medicaid NYRx also covers certain over-the-counter (OTC) medications with a prescription from a healthcare provider. These OTC medications may include items such as allergy medications, pain relievers, and vitamins. Coverage for OTC medications is subject to the same formulary and prior authorization rules as prescription drugs.
Navigating the Medicaid NYRx System
Navigating Medicaid NYRx can sometimes be challenging, especially for new enrollees. Understanding the key components of the system, such as the formulary, prior authorization process, and participating pharmacies, is essential for accessing needed medications. Beneficiaries are encouraged to work closely with their healthcare providers and pharmacists to ensure they receive the most appropriate and cost-effective treatment.
One of the first steps in navigating the system is to find a participating pharmacy. Medicaid NYRx has a network of pharmacies throughout New York State that accept Medicaid. Beneficiaries can use the online provider directory or contact their Medicaid managed care organization to find a pharmacy near them. It’s also important to confirm that the pharmacy is in-network before filling a prescription to avoid unexpected out-of-pocket costs.
When a healthcare provider prescribes a medication, it’s crucial to check whether the drug is on the Medicaid NYRx formulary. If the medication is not on the formulary, the provider may need to request prior authorization. The provider will submit a request to Medicaid NYRx, providing justification for why the medication is medically necessary. Medicaid NYRx will review the request and make a decision based on clinical guidelines and program policies.
Recent Changes and Updates to Medicaid NYRx
Medicaid NYRx is subject to ongoing changes and updates to ensure its effectiveness and sustainability. These changes may include revisions to the formulary, modifications to the prior authorization process, and adjustments to reimbursement rates for pharmacies. Staying informed about these changes is crucial for both beneficiaries and healthcare providers.
One recent change to Medicaid NYRx involves the implementation of new strategies to combat opioid abuse and misuse. The program has implemented stricter guidelines for prescribing opioid medications, including limits on the quantity and duration of prescriptions. These measures aim to reduce the risk of addiction and overdose while still ensuring that individuals with legitimate pain management needs have access to appropriate treatment.
Another significant update to Medicaid NYRx is the expansion of telehealth services. The program now covers telehealth visits for certain medical services, allowing beneficiaries to access care remotely. This is particularly beneficial for individuals who live in rural areas or have difficulty traveling to a healthcare provider’s office. Telehealth services can improve access to care and reduce healthcare costs.
Tips for Beneficiaries
To make the most of Medicaid NYRx benefits, beneficiaries should follow these tips:
- Stay informed about the Medicaid NYRx formulary and any changes to covered medications.
- Work closely with healthcare providers to choose medications that are both effective and cost-effective.
- Use a participating pharmacy to fill prescriptions.
- Understand the prior authorization process and be prepared to work with your healthcare provider to obtain necessary approvals.
- Keep your Medicaid card and other important documents in a safe place.
- Contact your Medicaid managed care organization or the New York State Department of Health with any questions or concerns.
The Future of Medicaid NYRx
The future of Medicaid NYRx is likely to be shaped by ongoing efforts to improve healthcare quality, control costs, and enhance access to care. As the healthcare landscape continues to evolve, Medicaid NYRx will need to adapt to meet the changing needs of its beneficiaries. This may involve exploring new models of care, leveraging technology to improve efficiency, and strengthening partnerships with healthcare providers and community organizations.
One potential area of focus for the future of Medicaid NYRx is the integration of behavioral health services. Mental health and substance use disorders are significant public health challenges, and Medicaid NYRx has a crucial role to play in ensuring that individuals with these conditions have access to appropriate treatment. By expanding coverage for behavioral health services and promoting integrated care models, Medicaid NYRx can help to improve outcomes and reduce the burden of these disorders.
Another area of potential growth for Medicaid NYRx is the use of data analytics to identify trends and improve program performance. By analyzing data on medication utilization, healthcare costs, and health outcomes, Medicaid NYRx can gain valuable insights into the effectiveness of its programs and policies. This information can be used to make data-driven decisions and implement targeted interventions to improve the health of beneficiaries.
In conclusion, Medicaid NYRx is a vital resource for ensuring access to prescription medications for eligible individuals in New York State. By understanding the program’s eligibility criteria, covered medications, and navigating the system effectively, beneficiaries can make the most of their benefits and improve their health outcomes. As Medicaid NYRx continues to evolve, it will be essential to stay informed about changes and updates to ensure that the program remains a valuable asset for the people of New York.
Medicaid NYRx provides a crucial safety net, ensuring that even the most vulnerable populations have access to life-saving and life-improving medications. The program’s success hinges on effective management, collaboration between stakeholders, and a commitment to continuous improvement. As New York State continues to address the healthcare needs of its residents, Medicaid NYRx will undoubtedly remain a cornerstone of its healthcare system. The ongoing efforts to refine and enhance Medicaid NYRx reflect a dedication to providing equitable and accessible healthcare for all New Yorkers, regardless of their financial circumstances.
For further information, beneficiaries and providers can consult the New York State Department of Health website or contact their managed care organization directly. Understanding the nuances of Medicaid NYRx empowers individuals to advocate for their health needs and navigate the healthcare system with confidence. [See also: Understanding Medicaid Eligibility in New York] [See also: Finding a Medicaid Provider in Your Area]
